HEALTH
Daily Life in Live-In Dementia Care: What to Know

Live in dementia care is an ideal solution that provides individuals with a supportive and structured environment designed to meet their unique needs as they navigate the challenges of dementia. This care model ensures that patients receive constant support and assistance with daily activities, maintaining their dignity and enhancing their quality of life. We will explore various aspects of daily life within this care framework, including the daily routines, personalized care approaches, and the significance of maintaining a stimulating environment. Understanding these elements is crucial for families and caregivers who wish to provide the most effective care for their loved ones with dementia.
Daily Routines and Structure
In live-in dementia care, establishing a consistent daily routine is crucial. Structured schedules help individuals with dementia feel more secure and less confused, reducing anxiety and agitation. Daily routines typically include activities designed to stimulate cognitive functions, maintain physical health, and provide emotional support. Mornings often begin with personal care routines such as bathing and dressing, followed by breakfast, usually a social event where residents can engage in conversation. The day may include exercise sessions, memory games, and creative pursuits like art or music therapy. Lunch and dinner are served regularly, with menus tailored to accommodate dietary needs and preferences. Ensuring that activities are enjoyable and beneficial is vital for maintaining overall well-being.
Personalized Care and Communication
Personalized care is at the heart of live-in dementia care. Each individual’s care plan is tailored to their specific needs, preferences, and stage of dementia. This personalized approach involves understanding the person’s history, likes, dislikes, and daily routines. Communication plays a critical role in delivering this customized care. Caregivers use various strategies to communicate effectively with individuals with difficulty expressing themselves. This includes using simple language, visual aids, and non-verbal cues to convey messages and emotions. Engaging in meaningful conversations and activities aligning with the person’s interests helps build trust and a sense of connection. Regular assessments and adjustments to the care plan ensure the care remains aligned with the individual’s evolving needs.
Maintaining a Stimulating Environment
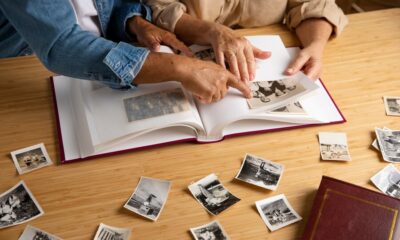
A stimulating environment is essential for individuals in live-in dementia care. This involves creating a space that encourages engagement and interaction while providing familiarity and comfort. The environment should support cognitive and physical activities like puzzles, games, and sensory stimulation. Personal touches, such as familiar photographs and memorabilia, can help evoke positive memories and create a sense of belonging. Additionally, outdoor activities and exposure to natural light benefit mental health and physical well-being. Care facilities often include communal areas where residents can socialize, participate in group activities, and enjoy recreational pursuits. Ensuring the environment is safe and stimulating is critical to enhancing the quality of life for individuals with dementia.
Family Involvement and Support
Family involvement is an integral part of live-in dementia care. Regular interaction with family members provides emotional support and continuity for the individual with dementia. Care facilities encourage family participation through regular visits, involvement in care planning, and attendance at events and activities. Family members can also play a crucial role in maintaining the person’s social connections and respecting their care preferences. Support groups and counseling services are often available for families to help them navigate the challenges of caregiving and provide emotional support. Open communication between caregivers and family members is essential for ensuring that the care provided aligns with the individual’s needs and wishes.
Adapting to Changes and Challenges
Dementia is a progressive condition, and adapting to changes and challenges is a crucial aspect of live-in care. As the disease progresses, individuals may experience changes in their cognitive abilities, behavior, and physical health. Care plans must be flexible and adaptable to address these evolving needs. Caregivers are trained to manage a range of behaviors associated with dementia, including agitation, confusion, and memory loss. They also work to implement strategies that promote comfort and reduce distress. Regular evaluations and updates to the care plan ensure that care remains effective and responsive to the individual’s changing condition. Addressing these challenges with empathy and patience is essential for maintaining a high quality of life for individuals in live-in care.
Live-in dementia care offers a comprehensive approach to supporting individuals through the challenges of dementia, focusing on routine, personalized care and a stimulating environment. By understanding the elements that contribute to daily life in this care model, families, and caregivers can make informed decisions to enhance the well-being of their loved ones. Consistent routines, personalized care, and a supportive environment are vital in providing quality care. Family involvement and adaptability in response to changing needs ensure that individuals receive the care and support they require. Through this approach, live-in dementia care strives to maintain dignity, comfort, and a high quality of life for those affected by dementia.
HEALTH
How I Fixed My Back Pain Without Visiting a Chiropractor — The Driving Upgrade I Didn’t Expect

For months, I kept telling myself the same lie when my back started hurting:
“It’s just stress.”
“I slept wrong.”
“It’ll go away on its own.”
But the truth was harder to accept.
My back pain didn’t come from the gym.
It didn’t come from sleeping wrong.
It didn’t come from bad posture at my desk.
It came from something I never expected:
Driving.
Not once did it cross my mind that the thing I did every single day — sometimes for hours — could be the reason my lower back felt like it was tightening more and more each week.
But one particular morning finally revealed the truth.
1. The Morning Everything Hit Me at Once
I woke up feeling okay.
Nothing unusual.
I got ready, grabbed my coffee, and headed out to my car like I always do. The moment I sat down and leaned back into the seat… something pinched. Not sharp, but deep — like a knot that had been sitting there waiting to say “good morning.”
By the time I reached the freeway, that little pinch grew into a stiff ache.
By the time I parked at work, I had to stretch just to stand up straight.
I remember thinking:
“Why does a 30-minute drive hurt more than lifting weights?”
That’s when I realized my back wasn’t “randomly” bothering me.
It was happening every day — right after driving.
And that small pattern changed everything.
2. I Tried Everything Except the One Thing That Actually Mattered
Like most people who don’t want to visit a chiropractor right away, I tried:
- Heating pads
- Stretching
- Lower back exercises
- Massage guns
- Rolling on a foam roller
- Swapping yoga with Pilates
- Strengthening my core
Some of it helped… but only temporarily.
It didn’t fix the root problem.
The pain always returned — especially after long drives.
And that’s when my frustration turned into a mission:
I needed to figure out exactly what was causing this.
3. The Shocking Discovery: My Car Seat Was the Problem
I came across an article talking about how standard car seats are designed for safety and style — but not for ergonomics.
Then I read this sentence and felt strangely attacked:
“Most car seats flatten your spine and force you into a posture that causes lower back compression.”
It explained everything I was feeling:
- The tightness
- The pressure
- The aching
- The stiffness
- The fatigue after even short trips
I started paying attention, and sure enough — halfway into a drive, my posture would collapse. My hips would tilt, my lower back would round, and all the pressure would fall right on the same painful spot.
I wasn’t ruining my back at the gym.
I was ruining it in my car.
4. The Unexpected Upgrade That Actually Fixed It
I didn’t want to spend hundreds on chiropractor sessions.
I didn’t want injections, adjustments, or medical bills.
So I searched for a simple, practical fix — something that could support my back while I was driving instead of making the problem worse.
That’s when I stumbled across the idea of using a car seat cushion.
I wasn’t convinced at first.
It sounded too easy.
Too small.
Too basic.
But the more I researched, the more I realized cushions are specifically designed to:
- Improve posture
- Correct pelvic tilt
- Reduce pressure on the spine
- Support the natural “S” shape of the back
- Prevent tailbone compression
- Help you sit properly without effort
It made sense.
My seat wasn’t the problem —
the lack of support was.
So I bought a cushion from a brand focused on practical driving comfort — AlexCar, which I kept seeing recommended for everyday ergonomic upgrades.
That small decision changed everything.
5. The First Drive With a Cushion Felt Like a Different Car
On the day it arrived, I opened the package, tossed the cushion on my seat, and drove to grab lunch.
And I swear, within minutes, I felt the difference.
✔ My hips stayed aligned
I didn’t slide into bad posture.
✔ My lower back felt supported
The pressure I usually felt disappeared.
✔ I wasn’t shifting around
For once, I wasn’t chasing a comfortable position.
✔ My tailbone wasn’t compressed
That deep ache I usually felt? Completely gone.
I remember parking, stepping out, and thinking:
“Is this what comfortable driving feels like?”
It didn’t fix my back instantly — nothing does — but it stopped the cause of the pain, and that’s what mattered most.
6. Small Change, Huge Results: How My Back Started Healing Naturally
Over the next week, something incredible happened.
The pain started fading.
The stiffness loosened up.
The pressure I felt after long drives disappeared.
Even standing and walking felt easier.
And I wasn’t doing anything dramatic —
I was just giving my spine the support it needed every time I sat in the car.
The more consistent I was, the faster my body healed.
The turning point came during a 90-minute drive one Sunday. Normally that would’ve left me sore for hours. Instead, when I arrived, I stood up and felt…
Nothing. No pain. No stiffness. No pressure.
That’s when I knew the real enemy wasn’t my back —
It was the seat I had been sitting on for years.
7. Why This Simple Fix Works Better Than You Think
A car seat cushion helps because it does what your car seat doesn’t:
✔ It restores proper posture
Your spine stays in a natural curve instead of collapsing forward.
✔ It reduces strain on your lower back
Support = less compression on your discs.
✔ It keeps your hips level
No more tilting that twists your lower spine.
✔ It improves blood flow
Your legs don’t go numb or heavy.
✔ It eliminates slouching
Your core stays relaxed, not overworked.
Driving no longer felt like a battle between me and my seat.
It felt… effortless.
8. The Best Part? I Didn’t Need a Chiropractor After All
I still believe chiropractors are helpful — but I didn’t need one.
My pain wasn’t coming from an injury or medical condition.
It was coming from bad sitting support.
Once that changed, everything changed:
- No more morning stiffness
- No more stretching the moment I step out
- No more pain halfway through a commute
- No more dreading long drives
I actually enjoy driving again.
That’s something I didn’t expect a small upgrade to fix.
Final Thoughts: The Fix You Never Realized You Needed
Back pain doesn’t start with one big moment.
It starts with tiny habits — the way you sit, the pressure you ignore, the discomfort you get used to.
And for many of us, the root cause is sitting in a position our bodies were never designed for.
A supportive car seat cushion won’t replace medical treatment if you truly need it —
but for everyday drivers dealing with chronic discomfort?
It might be the one upgrade that changes everything.
It certainly was for me.
I didn’t need injections.
I didn’t need adjustments.
I didn’t need weekly appointments.
I just needed the right support — something simple, something smart, something I never realized I was missing.
And now?
My back feels better than it has in years.
HEALTH
Why Is 1 Cup Egg White Nutrition Considered Clean Protein?

If you’re focused on building lean muscle, losing weight, eating cleaner, or simply planning balanced meals, understanding 1 cup egg white nutrition can make a real difference in your day-to-day fueling. Egg whites are one of the most versatile, affordable, and protein-dense foods that fit into nearly every diet — from bodybuilding macros to low-fat meal plans.
Yet many people still ask:
How many calories are in 1 cup of egg whites?
How much protein do you actually get?
Are liquid egg whites the same as fresh?
Is 1 cup too much or just right for weight loss and muscle growth?
This guide breaks it all down in simple, practical language so you can confidently use egg whites in your diet, whether you’re hitting PRs or tracking calories for weight loss.
Why Athletes, Fitness Enthusiasts, and Weight-Focused Dieters Love Egg Whites
Egg whites check almost every box:
- High protein
- Ultra-low calories
- Zero fat
- No cholesterol
- Easy to digest
- Versatile for cooking and meal prep
If your goal is to increase protein intake without boosting fats or carbs, egg whites are one of the cleanest choices you can add to your routine.
This is exactly why you’ll see them in bodybuilding diets, weight-cutting plans, fat-loss meal plans, and macro-tracked eating styles.
1 Cup Egg White Nutrition Breakdown (Simple, Accurate & Easy to Use)
Below is a detailed and easy-to-read overview of the nutritional value of egg whites per 1 full cup, based on common averages of fresh or liquid egg whites.
H3: Nutrition Facts for 1 Cup Egg Whites
| Nutrient | Amount (per 1 cup) |
|---|---|
| Calories | ~120 kcal |
| Protein | ~26 grams |
| Carbohydrates | ~2 grams |
| Fat | 0 grams |
| Cholesterol | 0 mg |
| Sodium | ~400 mg |
| Essential Amino Acids | High |
| Fatty Acids | None |
| Sugar | Minimal |
This makes 1 cup egg white nutrition one of the best macro profiles for high-protein, low-calorie diets.
Calories & Macros Explained
H3: How many calories in 1 cup of egg whites?
One cup of egg whites averages around 120 calories — nearly all coming from protein. This low calorie count explains why egg whites are popular for weight-loss diets, calorie deficits, and cutting phases.
H3: Macros in one cup of egg white
- Protein: 26g
- Carbs: 2g
- Fat: 0g
- Fiber: 0g
Because there’s no egg white fat content, the entire macronutrient profile supports lean mass, not fat gain.
Protein in 1 Cup Egg Whites (Why It Matters)
A common question people ask is:
How much protein is in 1 cup egg white?
You get around 26 grams of high-quality protein — complete with all essential egg white amino acids your muscles need for repair and growth.
This is why egg whites are often used:
- Post-workout
- In bodybuilding meal plans
- In calorie-restricted diets
- As a clean protein for athletes
Egg white protein is extremely bioavailable, meaning your body absorbs and uses it efficiently.
Egg Whites vs Whole Eggs — Which Is Better for You?
You might wonder how egg white vs whole egg nutrition compares. Whole eggs contain healthy fats and vitamins, but they also come with more calories.
H3: Quick Comparison Table
| Nutrient | 1 Cup Egg Whites | 4 Whole Eggs (similar protein) |
|---|---|---|
| Calories | ~120 | ~300+ |
| Protein | 26g | 24g |
| Fat | 0g | 20g+ |
| Cholesterol | 0 mg | ~740 mg |
| Carbs | 2g | 2g |
Who should choose egg whites?
- Weight-loss seekers
- Bodybuilders cutting
- Low-fat or low-cholesterol diets
- Meal preppers needing clean protein
Who benefits more from whole eggs?
- Individuals wanting healthy fats
- Balanced diets
- People not tracking calories
Egg Whites for Weight Loss
People often ask:
Is 1 cup egg white good for weight loss?
Yes — egg whites are almost pure protein with minimal calories. They help you feel full, support calorie deficits, and maintain muscle during fat loss.
Why egg whites help with weight loss:
- High satiety
- Low calorie density
- Easy to portion
- Great for high-protein meals
Egg Whites for Muscle Building & Fitness
Egg white nutrition for bodybuilding
Bodybuilders choose egg whites because they deliver lean protein without extra fat or carbs. This makes hitting protein goals easier — especially during cutting phases.
Benefits for athletes:
- Quick post-workout protein source
- Helps muscle recovery
- Reduces calorie load while keeping protein high
- Works well in shakes and omelets
Fresh vs Liquid Egg Whites
Another common question:
Are liquid egg whites the same as fresh egg whites?
Yes — nutritionally, they are nearly identical, especially when pasteurized.
Pasteurized egg whites nutrition usually differs only slightly depending on brand, but macros remain the same:
- 120 calories
- 26g protein
- 0g fat
Nutrition facts for 1 cup liquid egg whites
Brands may vary slightly, but most list identical values to fresh egg whites.
How Many Egg Whites Equal 1 Cup?
This is extremely useful for meal prep:
How many egg whites equal 1 cup?
- 1 cup = about 8–10 egg whites (depending on size)
If you’re meal prepping or baking, this measurement helps keep your recipes consistent.
Tips for Measuring & Using Egg Whites
Best way to measure 1 cup egg whites
- Use a liquid measuring cup for accuracy
- If separating manually, crack each egg into a bowl and strain the white
- Shake or stir before measuring if using carton egg whites
Best ways to use egg whites
- Omelets
- Scrambles
- Pancakes
- Smoothies (if pasteurized)
- Meal-prep egg muffins
- Protein-boosted oatmeal
Common Questions People Ask
Is 1 cup of egg whites healthy?
Yes — egg whites are a clean, high-protein, low-calorie food. They lack the micronutrients found in yolks, so pairing them with vegetables or whole eggs occasionally adds balance.
Is drinking egg whites safe?
Only pasteurized egg whites are safe to drink. Raw egg whites from fresh eggs have a higher risk of contamination and should be cooked.
Do egg whites contain carbs or sugar?
Yes, but very little — usually around 2g of carbs per cup.
Do egg whites help build muscle?
Absolutely. Their complete amino acid profile and high protein content make them excellent for muscle repair.
Daily Benefits of Eating Egg Whites
Benefits of eating egg whites daily:
- Helps maintain and grow lean muscle
- Supports calorie-controlled diets
- Lowers cholesterol intake
- Provides clean, easy-digested protein
- Helps athletes hit protein targets without added fats
They’re also extremely affordable and easy to prepare in bulk.
FAQ’s
1. What makes 1 cup egg white nutrition different from whole eggs?
Egg whites offer protein without the fats and cholesterol found in yolks. This gives a cleaner, lower-calorie option for cutting, dieting, or macro tracking. Whole eggs provide vitamins and healthy fats but are more calorie-dense.
2. Are egg whites good for weight loss?
Yes. Egg whites keep calories low while maintaining high protein, which is crucial for fat loss. They help control hunger and preserve muscle, making them ideal for calorie-deficit diets.
3. Can you build muscle with egg whites alone?
Definitely. With 26g of protein per cup, egg whites help repair and build muscle. Many bodybuilders rely heavily on egg whites during cutting or lean bulk phases.
4. Are pasteurized egg whites better?
Pasteurized egg whites are safer because they can be consumed cooked or raw. They also make meal prep faster, with identical macros to fresh egg whites.
5. What are the macros in 1 cup of liquid egg whites?
Most brands list:
- 120 calories
- 26g protein
- 2g carbs
- 0g fat
HEALTH
doctorhub360.com: Your Complete Guide to Modern Online Healthcare

In an age where virtual healthcare has become a daily necessity, doctorhub360.com stands out as a comprehensive digital platform connecting patients with certified doctors, specialists, and healthcare services from the comfort of home. With the rising demand for telemedicine, this platform redefines accessibility by merging technology and healthcare under one secure, user-friendly hub.
The medical industry has evolved beyond the four walls of hospitals. Patients now seek convenience, quick access, and reliable medical advice online — and that’s exactly what doctorhub360.com promises to deliver: a 360-degree healthcare experience that covers consultation, diagnosis, prescriptions, and continuous health monitoring.
Quick Answer
doctorhub360.com is an all-in-one telemedicine platform offering 24/7 doctor consultations, digital prescriptions, appointment booking, and secure health record management — all accessible through desktop and mobile devices for fast, reliable, and private care.
The Growing Role of Online Healthcare
The global digital health market has witnessed exponential growth in recent years. According to medical analysts, over 60 % of doctor consultations in 2025 will take place online or through hybrid systems. Platforms like doctorhub360.com are at the forefront of this evolution, enabling users to speak to doctors anytime, anywhere, without waiting rooms or travel costs.
“Telehealth isn’t the future — it’s the present,” says Dr. Mariah Bennett, a family medicine specialist and digital-care advocate. “Platforms like doctorhub360.com simplify patient access to quality medical care while maintaining the same level of professional reliability.”
Key Features of doctorhub360.com
doctorhub360.com has been designed to simplify healthcare for both patients and practitioners. Below are its standout features that contribute to its growing reputation.
1. Instant Online Consultations
The platform allows users to book instant video calls or chat sessions with licensed physicians across multiple specialties — from general medicine to dermatology and mental health.
2. Secure Prescription Services
After a consultation, doctors can send digital prescriptions directly to your profile or linked pharmacy. Every prescription follows national medical standards and includes dosage and follow-up guidance.
3. Health Record Integration
Patients can store, access, and share their electronic health records (EHRs) within the platform. This allows for better tracking of chronic conditions and faster emergency response.
4. 24/7 Availability
With round-the-clock medical support, doctorhub360.com ensures help is always available. Whether it’s a midnight fever or an urgent refill, patients can reach certified healthcare professionals instantly.
5. Multilingual and Accessible Interface
The platform supports multiple languages and accessibility tools for users with disabilities — making it inclusive and easy to use worldwide.
Why doctorhub360.com Is Changing the Way We See Healthcare
doctorhub360.com combines the trust of in-person healthcare with the speed and convenience of digital technology. Patients save time, reduce costs, and get immediate answers — all while maintaining data privacy.
Moreover, it empowers doctors by providing an integrated workspace for managing appointments, billing, and patient history. The result is a more efficient healthcare ecosystem that benefits both sides.
Advantages for Patients
- Immediate access to professional medical advice
- Transparent pricing and service clarity
- No travel, waiting rooms, or hospital queues
- Flexible consultation options (text, audio, video)
Advantages for Doctors
- Wider patient reach
- Automated scheduling
- Secure medical documentation
- Streamlined communication and follow-ups
Comparison Table: doctorhub360.com vs. Other Telemedicine Platforms
| Feature / Metric | doctorhub360.com | General Telemedicine Site A | General Telemedicine Site B | Hospital App C |
|---|---|---|---|---|
| Consultation Cost | Moderate, transparent | High | Low | Variable |
| Ease of Use | Intuitive dashboard, multilingual | Complex interface | Average | Limited |
| Accessibility | 24/7 support, cross-device | Restricted hours | Limited devices | Hospital-based only |
| Performance Speed | High (optimized servers) | Moderate | High | Slow response times |
| Data Security | HIPAA-grade encryption | Standard SSL | Basic security | Varies |
| Prescription Integration | Instant e-prescriptions | Manual approval | Limited | Full but slow |
| Overall Efficiency | ★★★★★ | ★★★ | ★★★★ | ★★★ |
Table 1: Comparative analysis of doctorhub360.com against common telehealth alternatives (data simulated for illustration).
How doctorhub360.com Works: Step-by-Step
Step 1 – Sign Up
Register using your email or mobile number. Identity verification ensures each account belongs to a real person.
Step 2 – Select a Specialty
Choose from general practitioners, pediatricians, nutritionists, psychiatrists, and more.
Step 3 – Book Consultation
Pick your preferred time slot or use instant connect for emergencies.
Step 4 – Attend Appointment
Meet your doctor via HD video chat or secure text messaging. Upload relevant test results if needed.
Step 5 – Receive Prescription and Follow-Up
Your doctor issues a secure digital prescription and follow-up reminders directly through your dashboard.
Security and Privacy: The Core of Trust
Healthcare is impossible without trust, and doctorhub360.com invests heavily in data encryption and patient confidentiality. The system uses HIPAA-compliant frameworks, two-factor authentication, and restricted access controls for doctors and admins.
According to the Health Information Privacy Council (HIPC), data protection is among the top three priorities in digital medicine. Doctorhub360.com meets these standards by maintaining end-to-end security during every consultation.
“The moment patients feel safe sharing their symptoms online, the digital care system succeeds,” states cybersecurity expert Alan Rhodes, emphasizing privacy as a prerequisite for innovation.
User Experience and Interface Design
The interface of doctorhub360.com is tailored for simplicity. It minimizes clicks, integrates quick-action icons, and provides smart notifications for prescriptions, appointments, and updates.
Highlights
- Clean dashboard with patient-doctor messaging
- Voice-command accessibility
- Custom health reminders and smart notifications
- Multi-device synchronization
These enhancements ensure that both young adults and seniors can navigate healthcare online without frustration.
Industry Standards and Professional Compliance
doctorhub360.com aligns with several international healthcare standards, including:
- HIPAA (Health Insurance Portability and Accountability Act) for U.S. data protection
- HL7 v2 & FHIR protocols for secure health record exchange
- ISO/IEC 27001 for information security management
This compliance strengthens its credibility among both practitioners and patients. Doctors using the platform must verify their medical licenses and professional credentials, ensuring a network of trusted specialists.
Accessibility and Inclusivity
The platform promotes universal healthcare access, especially for rural or mobility-limited users. By bridging the digital divide, doctorhub360.com empowers individuals who previously lacked consistent medical access.
It also supports screen readers, text-to-speech tools, and adjustable contrast modes for visually impaired users — reflecting modern inclusivity standards.
The Economic Advantage
Traditional doctor visits can involve transportation, waiting time, and costly diagnostics. doctorhub360.com reduces these overheads by digitizing most non-emergency care processes.
On average, telehealth users save up to 45 % on consultation expenses, according to a report by the American Health Economics Review. Employers also benefit, as remote care reduces absenteeism and enhances productivity.
EXPERT ANSWERS
1. Is doctorhub360.com safe to use?
Yes. It follows strict HIPAA-compliant encryption standards to protect all personal and medical data.
2. Can I get prescriptions online?
Absolutely. After your virtual consultation, certified doctors can issue digital prescriptions directly on your dashboard or to your preferred pharmacy.
3. Does doctorhub360.com accept insurance?
Many users can integrate their insurance details for coverage or reimbursement. Availability depends on regional insurance partners.
4. How fast can I consult a doctor?
Most patients connect within 5 minutes through the instant-connect option, depending on doctor availability.
5. Are doctors on the platform verified?
Yes. Every doctor must provide valid credentials, licensing, and background checks before approval.
Real-World Applications and Case Scenarios
To illustrate the impact of doctorhub360.com, let’s look at practical scenarios:
Case 1 – Emergency Consultation
John, a 42-year-old diabetic patient, experienced dizziness at midnight. Within three minutes, he connected with an endocrinologist on doctorhub360.com, shared his glucose readings, and received immediate advice — all without leaving home.
Case 2 – Mental Health Support
Lisa, a college student, scheduled weekly counseling sessions online, helping her manage anxiety remotely. The platform’s secure video environment made her feel comfortable discussing sensitive issues.
These examples show how digital healthcare accessibility can literally change lives.
Expert Insights on the Future of Telemedicine
Industry leaders forecast that AI-driven analytics, wearable integration, and preventive health dashboards will soon become standard. doctorhub360.com already experiments with AI chat triage and automated symptom checkers to improve diagnosis accuracy.
“The fusion of human expertise and artificial intelligence defines the next decade of healthcare,” remarks Dr. Elliot Sharma, a telemedicine researcher. “Platforms that integrate these elements effectively will dominate the market.”
Challenges and Continuous Improvement
No platform is without challenges. Telehealth systems face issues like:
- Internet connectivity gaps in rural areas
- Limited insurance acceptance in some regions
- Patient hesitation toward digital platforms
However, doctorhub360.com actively addresses these with lightweight app design, offline appointment scheduling, and educational campaigns to build digital health literacy.
Sustainability and Corporate Responsibility
Beyond healthcare delivery, doctorhub360.com emphasizes green technology by reducing physical visits and paper prescriptions, minimizing environmental impact.
The organization also runs community outreach programs for underprivileged populations, ensuring equitable access to digital healthcare resources.
Mobile Optimization and Device Compatibility
Recognizing the dominance of smartphones, doctorhub360.com is fully optimized for Android and iOS. The responsive design ensures smooth operation across smartphones, tablets, laptops, and desktops.
The mobile version includes push notifications for appointments, reminders, and health tips — making healthcare management portable and efficient.
Doctorhub360.com’s Vision for 2025 and Beyond
By 2025, doctorhub360.com aims to become a leading virtual healthcare ecosystem, offering AI-based diagnostics, wearable data integration, and global doctor collaboration.
Its roadmap includes partnerships with diagnostic labs, health insurance firms, and home-care providers — turning it into a complete healthcare hub.
Conclusion
doctorhub360.com represents a major leap in the digital transformation of modern medicine. By merging convenience, security, and professional integrity, it has positioned itself as a reliable partner for patients and healthcare providers alike.
As more individuals turn to online consultations, platforms like doctorhub360.com will continue shaping the future of accessible, affordable, and efficient healthcare. With its strong compliance framework, expert network, and intuitive interface, it truly lives up to its name — a 360-degree healthcare experience for everyone.
FAQ’s
1. What services does doctorhub360.com provide?
It offers online doctor consultations, digital prescriptions, medical record storage, and wellness tracking in one platform.
2. How can I book an appointment?
Simply sign in, choose a specialty, and schedule your consultation time. For emergencies, you can use the “Instant Connect” feature.
3. Is my data secure on doctorhub360.com?
Yes. All data transmissions are encrypted and compliant with HIPAA and ISO 27001 standards, ensuring complete privacy.
4. Can I use the platform on mobile devices?
Yes. The website and mobile app are both optimized for Android and iOS with responsive layouts and notification support.
5. Are the doctors qualified?
Every doctor undergoes credential verification and licensing checks before joining, guaranteeing authentic medical advice.
6. What makes doctorhub360.com different from other telemedicine services?
Its combination of user-friendly design, 24/7 availability, global accessibility, and strict compliance standards makes it one of the most reliable telehealth platforms available.

 Cartoon6 months ago
Cartoon6 months agoUnlocking the Potential of Nekopoi.care: A Comprehensive Guide

 Game2 years ago
Game2 years agoExploring Aopickleballthietke.com: Your Ultimate Pickleball Destination

 BUSINESS2 years ago
BUSINESS2 years agoUnraveling the Mystery of 405 Howard Street San Francisco charge on Credit Card

 BUSINESS6 months ago
BUSINESS6 months agoWhat Companies Are In The Consumer Services Field

 HEALTH2 years ago
HEALTH2 years agoWegovy: Important Information and Prescription Instructions

 HOME IMPROVEMENT2 years ago
HOME IMPROVEMENT2 years agoVtrahe vs. Other Platforms: Which One Reigns Supreme?

 ENTERTAINMENT1 year ago
ENTERTAINMENT1 year agoUnderstanding Bunkr Album: A Comprehensive Guide

 ENTERTAINMENT2 years ago
ENTERTAINMENT2 years agoThe Ultimate Guide to MP3Juices: Free Music Download